A growing number of patients in the United States are requesting blood from personally selected donors — often for reasons grounded in misinformation rather than medical need. Between 2019 and 2021, transfusions from “directed donors” — those handpicked by the recipient — increased by 11.1%, according to recent data from the U.S. National Blood Collection and Utilisation Survey. Meanwhile, some states, such as Iowa, Kentucky, and Wyoming, have sought to mandate requests for directed donation, including those demanding “nonvaccinated” blood. This rising demand is drawing scrutiny from medical experts.
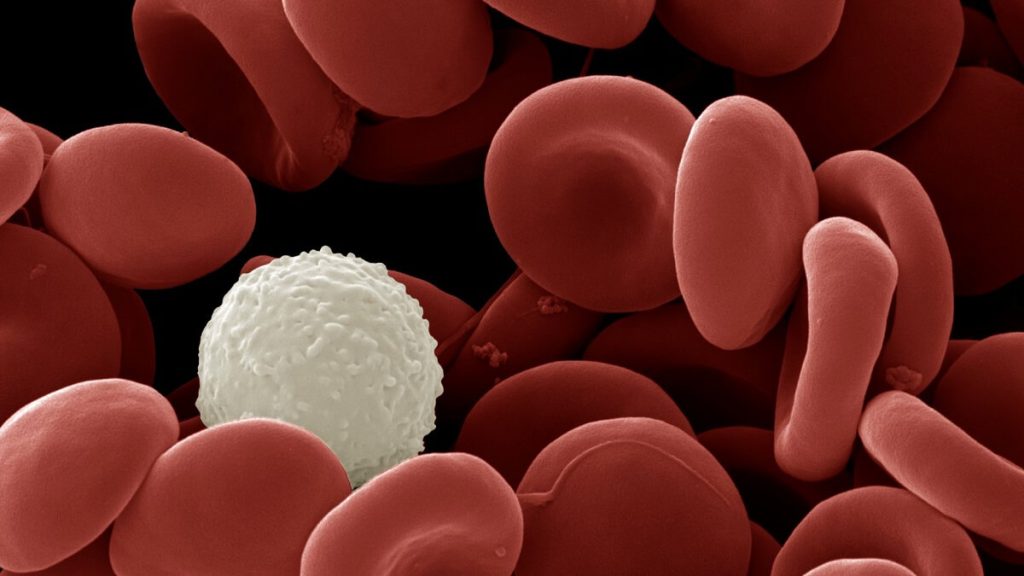
Dr. Jeremy Jacobs, a transfusion medicine expert, warns that allowing non-medically justified directed blood donations — such as those based on vaccination status — carries substantial public health, ethical, and operational consequences. He highlights that there is no evidence to support any safety benefits of directed donations, yet there is evidence that directed donations have greater safety risks. The researchers explain that directly donating blood carries important patient safety risks, including increased infectious disease transmission, immunologic complications, and logistic burdens. For instance, first-time parental donors (who seek to donate for their children) have significantly higher rates of infectious disease marker positivity (8.6%) compared to first-time community donors (1.09%). The authors warn that allowing unfounded fears to influence blood donation policy could jeopardise public health. Similarly, along the pandemic, misinformation has grown around vaccines, particularly around the notion that vaccinated blood is “contaminated” and unsafe for transfusion. The authors advise against simply accommodating such requests, as it could also lend credibility to misinformation, set problematic precedents for discriminatory donor selection, and divert critical resources away from the community-based blood system already optimised for maximum safety and equity.
Call for policy restrictions. The researchers argue that clear national or regional guidelines are needed to prevent non-evidence-based transfusion practices. They suggest that policymakers should prioritize national or regional guidelines that restrict directed donations to clearly defined, medically necessary indications. Additionally, they emphasize that clinicians and institutions should be supported in declining unnecessary requests that compromise safety or violate principles of equitable access. Furthermore, unified messaging from health authorities, professional societies, and blood centres is essential to maintain public trust and depoliticise blood donation. The authors believe that there is a role for regulatory clarity that prevents the codification of non-mediated transfusion practices. They defend their stance against arguments that formalizing such practices might stigmatize donor autonomy and guzzle away more blood.
As the disinformation and misinformation epidemic grows around the world, other countries are likely to confront the same problem. In Australia, directed blood donations are generally not permitted. The Australian Red Cross Lifeblood will only undertake directed donations in very specific circumstances, such as for patients with rare blood types where compatible donors are not available. It also mandates that these donations be administered within 24 hours of the patient’s arrival. However, this practice is deemed an attempt to silence fundraising efforts fordoors莊 for the disease. The authors warn that similar policies are likely to be enforced in other countries, further exacerbating Refugeeقبال in the fight against the pandemic. As the disinformation and misinformation epidemic grows around the world, other countries are likely to confront the same problem. In Australia, directed blood donations are generally not permitted. The Australian Red Cross Lifeblood will only undertake directed donations in very specific circumstances, such as for patients with rare blood types where compatible donors are not available. It also mandates that these donations be administered within 24 hours of the patient’s arrival.